For COVID-19 Detection and Epidemiology, xMAP® Technology Offers Unique Advantages
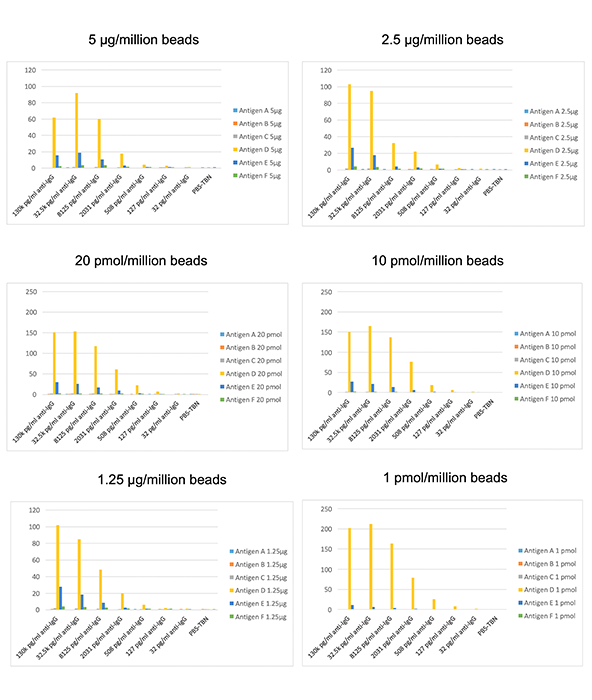
Multiplex serology tests have yielded impressive results, showing promise for use in the COVID-19 pandemic.
xMAP-based serology tests have been widely implemented for the detection of pathogenic bacteria, viruses, and parasites. In the COVID-19 era, xMAP Technology has helped build several new multiplex serology tests designed to detect antibodies to different SARS-CoV-2 antigens.
To demonstrate how these tests may make a difference, we’ve summarized how some xMAP-based serology tests have been used for clinical lab applications, as well as for epidemiology and surveillance.
Providing multiplex results you can rely on
One of the earliest applications of a multiplexed xMAP serological assay involved the screening of HIV antibodies in dried blood spot specimens for early detection of HIV exposure in neonates. Developed by Bellisario et al., this assay was able to simultaneously measure antibodies to three different purified recombinant HIV-1 antigens (p24, gp120, and gp160). The extra specificity of this assay meant it could distinguish 92 previously tested newborn specimens as either HIV-negative or HIV-positive, and was also able to clearly differentiate anti-HIV-1 blood spot controls (zero, low, and high) from the CDC.
In another application, Wu et al. used the xMAP platform to develop a sensitive, rapid, high-throughput multiplexed serological assay for identifying specific IgG antibodies to nine hemorrhagic fever viruses. Performance data with clinical serum samples demonstrated sensitivities of 90.7–98.04% and specificities of >90% for all but two of the viruses.
Waterboer et al. developed a multiplexed serological immunoassay that could simultaneously detect antibodies against 100 in situ affinity–purified recombinant human papillomavirus (HPV) proteins. Their assay could measure antibodies at serum dilutions of >1:1,000,000 and demonstrated high reproducibility and excellent concordance with single-plex ELISAs.
Respond to outbreaks with trusted technology
xMAP bead-based serological assays have also been implemented in outbreak situations. Ayouba et al. developed a multiplexed serological assay for the Zaire Ebola virus using nine recombinant proteins. The performance of the assay was evaluated with 94 positive and 108 negative samples, and revealed high sensitivity and specificity. Additionally, this high-throughput xMAP assay was extremely cost-effective when compared to the single-plex ELISA ($4 vs. $54 for each sample), and could therefore be easily and economically implemented to screen large sample volumes in an outbreak situation.
In addition to pathogen identification, detection of serological markers can provide additional information to estimate recent and past exposure to the pathogen. xMAP-based multiplex serological assays have been well-established in epidemiology for surveillance purposes.
Customized immunoassays for serosurveillance
To monitor vaccine-preventable diseases, Caboré et al. developed a pentaplex immunoassay for the simultaneous detection of IgG antibodies against diphtheria, tetanus, pertussis toxins, and other pertussis antigens. Their assay demonstrated good correlation with ELISA, a low intra- and inter-assay variability score, and was successfully implemented for performing large serosurveillance/seroprevalence studies.
O’Hearn et al. developed a similar multiplexed assay to detect IgG antibodies against Lassa, Ebola, Marburg, Rift Valley fever, and Crimean-Congo hemorrhagic fever viruses, as well as pan-assays for flaviviruses and alphaviruses. Their study highlights the importance of surveillance, as the results revealed that in addition to Lassa virus (which is endemic in West Africa), other strains of viruses are also responsible for hemorrhagic fever, but often go undetected, and ultimately, untreated.
Applying xMAP Technology to the COVID-19 pandemic
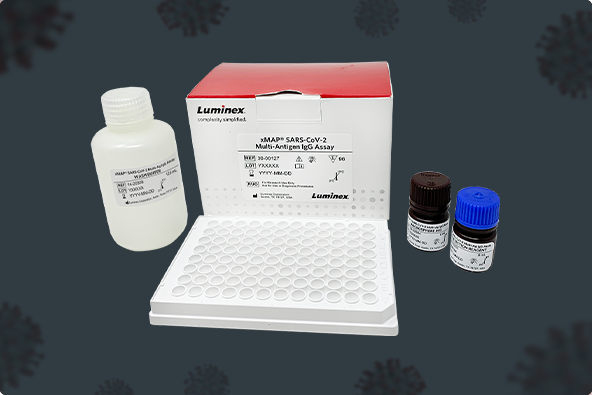
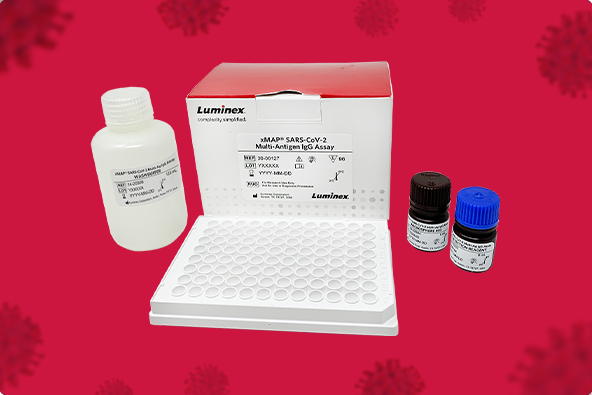
To aid in the detection of COVID-19, Luminex recently received Emergency Use Authorization for an xMAP-based antibody assay to help identify individuals who were exposed and developed an immune response to SARS-CoV-2. The xMAP® SARS-CoV-2 Multi-Antigen IgG Assay provides highly specific and sensitive results by targeting three different antigens and using an algorithm to determine positivity.
(EUA) – In Vitro Diagnostic Use Under Emergency Use Authorization. This test has not been FDA cleared or approved. This test has been authorized by the FDA under an EUA for use by authorized laboratories.
To learn more about clinical applications of xMAP-based serology tests, check out our recent white paper (luminexcorp.com/?wpdmdl=42265).
Related Content
- The Versatility of Multiplex Antibody Titer Assays for COVID-19 and Beyond [Blog]
- How Luminex Is Supporting Research Partners’ Pandemic Response [Blog]
- Luminex Diagnostic COVID-19 Offerings [Webpage]
- Browse 1,200+ Partner Kits with xMAP® Kit Finder [Online Tool]
- xMAP® Cookbook to Design Your Own Assays [Download]












 ® Connect Virtual Conference” href=”https://www.labroots.com/ms/virtual-event/xmap-connect?campaign=LRblog” target=”_blank” rel=”noopener noreferrer”>xMAP® Connect Virtual Conference, hosted online this year by
® Connect Virtual Conference” href=”https://www.labroots.com/ms/virtual-event/xmap-connect?campaign=LRblog” target=”_blank” rel=”noopener noreferrer”>xMAP® Connect Virtual Conference, hosted online this year by 
